Fraud, Waste & Abuse
Fraud
“The obtaining of a benefit through the intentional misrepresentation or concealment of material facts.”
Waste
“The incurring of unnecessary costs as a result of deficient management, practices, or controls.”
Abuse
“The excessive or improper using of government resources.”
One of the most important roles a person can play in combating fraud, waste, and abuse is to take the initiative to report these activities. An individual reporting fraud may be entitled to reward under RSMo. 191.907.
Fraud, Waste, or Abuse may be committed by a Medicaid Provider and/or a Medicaid Recipient.
Provider Fraud
A Medicaid (Mo HealthNet) Provider is a person or entity that performs or bills for medical services rendered to Medicaid participants. Medicaid Fraud by a provider impacts Missouri taxpaying citizens whose tax dollars are being subjected to fraud, waste, and abuse. Medicaid fraud also affects participants whose benefits are governed by dollars available and providers whose professions are impacted by the effects of others’ abuse.
Provider fraud is generally the result of an intentional misrepresentation of services rendered. While the fraud, waste and abuse may take on many forms, some of the more common are:
- Billing for services when no service was provided (“phantom billing”).
- Billing for a more expensive treatment or service than was actually provided (“upcoding”).
- Billing for unnecessary services.
- Billing for the same service multiple times.
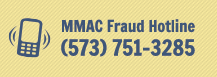
To report Medicaid Provider fraud, use one of the following options:
- Call the MMAC Fraud Hotline: (573) 751-3285
- Email the MMAC Fraud Email: MMAC.ReportFraud@dss.mo.gov
Participant Fraud
Public Assistance Programs such as Temporary Assistance for Needy Families (TANF), Supplemental Nutrition Assistance Program (SNAP or Food Stamps), and Energy Assistance may be provided to qualified participants to help in difficult times. Reporting suspected fraud in these programs is a responsibility of every Missourian.
Participant fraud is generally the result of an intentional misrepresentation on an application in order to qualify for public assistance benefits or receive more benefits than allowed. Common examples of participant fraud include:
- Making a false written or oral statement on an application regarding one’s earned income, resources or job status.
- Making a false written or oral statement on an application regarding one’s household composition.
- Making a false written or oral statement on an application regarding your residency.
To report Public Assistance fraud, use one of the following options:
- Call: (877) 770-8055
- Email: DLS.ReportFraud@dss.mo.gov
- Complete: Missouri Public Assistance Fraud Form
What Can I Do as a Provider?
The provider’s role in the billing process is often critical to ensuring fraud is not occurring. Simply hiring a billing agency does not negate the provider’s responsibility to ensure proper billing is occurring. Providers are encouraged to work closely with those billing on their behalf to verify the appropriateness and validity of claims submitted.
What Can I Do as a Participant?
Participants can assist in combating fraud by guarding their MO HealthNet Identification Number and personal information. A participant who allows another individual to use their card is aiding in the commission of fraud and is subject to the same prosecutorial possibility as the individual who actually used the card. A participant should also ensure they protect any medications from theft, and if theft occurs, report it to the appropriate authorities. Under no circumstance should participants obtain unnecessary medications, or take no longer needed medications, and sell them to other individuals.
